Diabetes
Diabetes is a disorder in which blood sugar (glucose) levels are abnormally high because the body does not produce enough insulin to meet its needs. Diabetes affects the amount of sugar in the blood. There are many types of sugar. Some sugars are simple, and others are more complex. Table sugar (sucrose) is made of two simpler sugars called glucose and fructose. Milk sugar (lactose) is made of glucose and a simple sugar called galactose. The carbohydrates in bread, pasta, rice, and similar foods are long chains of different simple sugar molecules. Sucrose, lactose, carbohydrates, and other complex sugars must be broken down into their component simple sugars by enzymes in the digestive tract before the body can absorb them. Once the body absorbs simple sugars, it usually converts them all into glucose, which is the main source of fuel for the body. Glucose is the sugar that is transported through the bloodstream and taken up by cells. Blood "sugar" really means blood glucose.
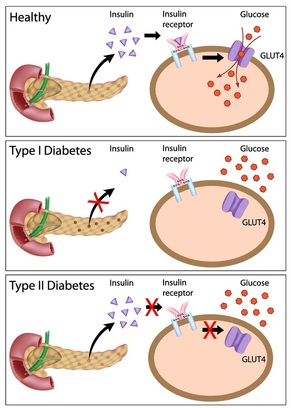
Insulin, a hormone released from the pancreas, controls the amount of glucose in the blood. Glucose in the bloodstream stimulates the pancreas to produce insulin. Insulin allows glucose to move from the blood into the cells. Once inside the cells, glucose is converted to energy, which is used immediately, or the glucose is stored as fat or glycogen until it is needed.
If the body does not produce enough insulin to move the glucose into the cells, or if the cells stop responding normally to insulin, the resulting high levels of glucose in the blood and the inadequate amount of glucose in the cells together produce the symptoms and complications of diabetes.
Types
Prediabetes
Prediabetes is a condition in which blood glucose levels are too high to be considered normal but not high enough to be labeled diabetes. People have prediabetes if their fasting blood glucose level is between 101 mg/dL and 126 mg/dL or if their blood glucose level 2 hours after a glucose tolerance test is between 140 mg/dL and 200 mg/dL. Identifying people with prediabetes is important because the condition carries a higher risk for future diabetes as well as heart disease.
Type 1 Diabetes Mellitus
In type 1 diabetes, more than 90% of the insulin-producing cells of the pancreas are permanently destroyed. The pancreas, therefore, produces little or no insulin. Only about 10% of all people with diabetes have type 1 disease. Most people who have type 1 diabetes develop the disease before age 30, although it can develop later in life. Scientists believe that an environmental factor—possibly a viral infection or a nutritional factor during childhood or early adulthood—causes the immune system to destroy the insulin-producing cells of the pancreas. A genetic predisposition may make some people more susceptible to the environmental factor.
Type 2 Diabetes Mellitus
In type 2 diabetes the pancreas continues to produce insulin, sometimes even at higher-than-normal levels. However, the body develops resistance to the effects of insulin, so there is not enough insulin to meet the body's needs. Type 2 diabetes was once rare in children and adolescents but has recently become more common. However, it usually begins in people older than 30 and becomes progressively more common with age. About 27% of people older than 65 have type 2 diabetes. People of certain racial and ethnic backgrounds are at increased risk of developing type 2 diabetes: African Americans, American Indians, and Hispanics who live in the United States have a twofold to threefold increased risk. Type 2 diabetes also tends to run in families. Obesity is the chief risk factor for developing type 2 diabetes, and 80 to 90% of people with this disorder are overweight or obese. Because obesity causes insulin resistance, obese people need very large amounts of insulin to maintain normal blood glucose levels.
Symptoms
The two types of diabetes have very similar symptoms. The first symptoms are related to the direct effects of high blood glucose levels. When the blood glucose level rises above 160 to 180 mg/dL, glucose spills into the urine. When the level of glucose in the urine rises even higher, the kidneys excrete additional water to dilute the large amount of glucose. Because the kidneys produce excessive urine, people with diabetes urinate large volumes frequently (polyuria). The excessive urination creates abnormal thirst (polydipsia). Because excessive calories are lost in the urine, people may lose weight. To compensate, people often feel excessively hungry. Other symptoms include blurred vision, drowsiness, nausea, and decreased endurance during exercise.
In people with type 1 diabetes, the symptoms often begin abruptly and dramatically. A condition called diabetic ketoacidosis may quickly develop. Without insulin, most cells cannot use the glucose that is in the blood. The initial symptoms of diabetic ketoacidosis include excessive thirst and urination, weight loss, nausea, vomiting, fatigue, and—particularly in children—abdominal pain. Breathing tends to become deep and rapid as the body attempts to correct the blood's acidity. The breath smells like acetone because of the smell of the ketones escaping into the breath. Without treatment, diabetic ketoacidosis can progress to coma and death, sometimes very quickly.
People with type 2 diabetes may not have any symptoms for years or decades before they are diagnosed. Symptoms may be subtle. Increased urination and thirst are mild at first and gradually worsen over weeks or months. Eventually, people feel extremely fatigued, are likely to develop blurred vision, and may become dehydrated.
Because people with type 2 diabetes produce some insulin, ketoacidosis does not usually develop even when type 2 diabetes is untreated for a long time. However, the blood glucose levels can become extremely high (often exceeding 1,000 mg/dL). Such high levels often happen as the result of some superimposed stress, such as an infection or drug use. When the blood glucose levels get very high, people may develop severe dehydration, which may lead to mental confusion, drowsiness, and seizures, a condition called nonketotic hyperglycemic-hyperosmolar syndrome. Currently, many people with type 2 diabetes are diagnosed by routine blood glucose testing before they develop such severely high blood glucose levels.
Complications
People with diabetes may experience many serious, long-term complications. Some of these complications begin within months of the onset of diabetes, although most tend to develop after a few years. Most of the complications gradually worsen. In people with diabetes, strictly controlling the levels of glucose in the blood makes these complications less likely to develop or worsen.
Over time, elevated levels of glucose in the blood and poor circulation can harm the heart, brain, legs, eyes, kidneys, nerves, and skin, resulting in angina, heart failure, strokes, leg cramps during walking (claudication), poor vision, kidney failure, damage to nerves (neuropathy), and skin breakdown. Poor circulation to the skin can lead to ulcers and infections and causes wounds to heal slowly. People with diabetes are particularly likely to have ulcers and infections of the feet and legs. Too often, these wounds heal slowly or not at all, and amputation of the foot or part of the leg may be needed. People with diabetes often develop bacterial and fungal infections, typically of the skin. When the levels of glucose in the blood are high, white blood cells cannot effectively fight infections. Any infection that develops tends to be more severe and takes longer to resolve.
Damage to the blood vessels of the eye can cause loss of vision (diabetic retinopathy). The kidneys can malfunction, resulting in kidney failure that may require dialysis or kidney transplantation. Doctors usually check the urine of people with diabetes for abnormally high levels of protein (albumin), which is an early sign of kidney damage. Damage to nerves can manifest in several ways. If a single nerve malfunctions, an arm or leg may suddenly become weak. If the nerves to the hands, legs, and feet become damaged (diabetic polyneuropathy), sensation may become abnormal, and tingling or burning pain and weakness in the arms and legs may develop. Damage to the nerves of the skin makes repeated injuries more likely because people cannot sense changes in pressure or temperature.
If you think you may have diabetes, please contact Dr. Linda Gedeon for proper evaluation and to discuss the best treatment options for you.
Insulin, a hormone released from the pancreas, controls the amount of glucose in the blood. Glucose in the bloodstream stimulates the pancreas to produce insulin. Insulin allows glucose to move from the blood into the cells. Once inside the cells, glucose is converted to energy, which is used immediately, or the glucose is stored as fat or glycogen until it is needed.
If the body does not produce enough insulin to move the glucose into the cells, or if the cells stop responding normally to insulin, the resulting high levels of glucose in the blood and the inadequate amount of glucose in the cells together produce the symptoms and complications of diabetes.
Types
Prediabetes
Prediabetes is a condition in which blood glucose levels are too high to be considered normal but not high enough to be labeled diabetes. People have prediabetes if their fasting blood glucose level is between 101 mg/dL and 126 mg/dL or if their blood glucose level 2 hours after a glucose tolerance test is between 140 mg/dL and 200 mg/dL. Identifying people with prediabetes is important because the condition carries a higher risk for future diabetes as well as heart disease.
Type 1 Diabetes Mellitus
In type 1 diabetes, more than 90% of the insulin-producing cells of the pancreas are permanently destroyed. The pancreas, therefore, produces little or no insulin. Only about 10% of all people with diabetes have type 1 disease. Most people who have type 1 diabetes develop the disease before age 30, although it can develop later in life. Scientists believe that an environmental factor—possibly a viral infection or a nutritional factor during childhood or early adulthood—causes the immune system to destroy the insulin-producing cells of the pancreas. A genetic predisposition may make some people more susceptible to the environmental factor.
Type 2 Diabetes Mellitus
In type 2 diabetes the pancreas continues to produce insulin, sometimes even at higher-than-normal levels. However, the body develops resistance to the effects of insulin, so there is not enough insulin to meet the body's needs. Type 2 diabetes was once rare in children and adolescents but has recently become more common. However, it usually begins in people older than 30 and becomes progressively more common with age. About 27% of people older than 65 have type 2 diabetes. People of certain racial and ethnic backgrounds are at increased risk of developing type 2 diabetes: African Americans, American Indians, and Hispanics who live in the United States have a twofold to threefold increased risk. Type 2 diabetes also tends to run in families. Obesity is the chief risk factor for developing type 2 diabetes, and 80 to 90% of people with this disorder are overweight or obese. Because obesity causes insulin resistance, obese people need very large amounts of insulin to maintain normal blood glucose levels.
Symptoms
The two types of diabetes have very similar symptoms. The first symptoms are related to the direct effects of high blood glucose levels. When the blood glucose level rises above 160 to 180 mg/dL, glucose spills into the urine. When the level of glucose in the urine rises even higher, the kidneys excrete additional water to dilute the large amount of glucose. Because the kidneys produce excessive urine, people with diabetes urinate large volumes frequently (polyuria). The excessive urination creates abnormal thirst (polydipsia). Because excessive calories are lost in the urine, people may lose weight. To compensate, people often feel excessively hungry. Other symptoms include blurred vision, drowsiness, nausea, and decreased endurance during exercise.
In people with type 1 diabetes, the symptoms often begin abruptly and dramatically. A condition called diabetic ketoacidosis may quickly develop. Without insulin, most cells cannot use the glucose that is in the blood. The initial symptoms of diabetic ketoacidosis include excessive thirst and urination, weight loss, nausea, vomiting, fatigue, and—particularly in children—abdominal pain. Breathing tends to become deep and rapid as the body attempts to correct the blood's acidity. The breath smells like acetone because of the smell of the ketones escaping into the breath. Without treatment, diabetic ketoacidosis can progress to coma and death, sometimes very quickly.
People with type 2 diabetes may not have any symptoms for years or decades before they are diagnosed. Symptoms may be subtle. Increased urination and thirst are mild at first and gradually worsen over weeks or months. Eventually, people feel extremely fatigued, are likely to develop blurred vision, and may become dehydrated.
Because people with type 2 diabetes produce some insulin, ketoacidosis does not usually develop even when type 2 diabetes is untreated for a long time. However, the blood glucose levels can become extremely high (often exceeding 1,000 mg/dL). Such high levels often happen as the result of some superimposed stress, such as an infection or drug use. When the blood glucose levels get very high, people may develop severe dehydration, which may lead to mental confusion, drowsiness, and seizures, a condition called nonketotic hyperglycemic-hyperosmolar syndrome. Currently, many people with type 2 diabetes are diagnosed by routine blood glucose testing before they develop such severely high blood glucose levels.
Complications
People with diabetes may experience many serious, long-term complications. Some of these complications begin within months of the onset of diabetes, although most tend to develop after a few years. Most of the complications gradually worsen. In people with diabetes, strictly controlling the levels of glucose in the blood makes these complications less likely to develop or worsen.
Over time, elevated levels of glucose in the blood and poor circulation can harm the heart, brain, legs, eyes, kidneys, nerves, and skin, resulting in angina, heart failure, strokes, leg cramps during walking (claudication), poor vision, kidney failure, damage to nerves (neuropathy), and skin breakdown. Poor circulation to the skin can lead to ulcers and infections and causes wounds to heal slowly. People with diabetes are particularly likely to have ulcers and infections of the feet and legs. Too often, these wounds heal slowly or not at all, and amputation of the foot or part of the leg may be needed. People with diabetes often develop bacterial and fungal infections, typically of the skin. When the levels of glucose in the blood are high, white blood cells cannot effectively fight infections. Any infection that develops tends to be more severe and takes longer to resolve.
Damage to the blood vessels of the eye can cause loss of vision (diabetic retinopathy). The kidneys can malfunction, resulting in kidney failure that may require dialysis or kidney transplantation. Doctors usually check the urine of people with diabetes for abnormally high levels of protein (albumin), which is an early sign of kidney damage. Damage to nerves can manifest in several ways. If a single nerve malfunctions, an arm or leg may suddenly become weak. If the nerves to the hands, legs, and feet become damaged (diabetic polyneuropathy), sensation may become abnormal, and tingling or burning pain and weakness in the arms and legs may develop. Damage to the nerves of the skin makes repeated injuries more likely because people cannot sense changes in pressure or temperature.
If you think you may have diabetes, please contact Dr. Linda Gedeon for proper evaluation and to discuss the best treatment options for you.